
In the last two decades there has been increasing interest in biological grafts, the properties of natural and synthetic substitutes, and how alternatives to the traditional iliac crest autologous graft harvest can be safely used to accelerate healing and fusion. The ACDF procedure was first described by Cloward 2 and Smith & Robinson 3 six decades ago using autologous iliac crest bone graft (ICBG) and a lot has changed since. 1 Current technological advances in biomaterials are shaping the future of surgical techniques. Anterior cervical discectomy and fusion (ACDF) interventions have doubled over the previous decades and this trend is likely to continue as the population ages. Keywords: cost-effectiveness, i-factor, spine fusion, spine allograft, cervical spondylosis, anterior cervical discectomy and fusion, cost analysis, decision analysisĬervical spondylosis is the most common cause of myelopathy and upper extremity radiculopathy. In a threshold sensitivity analysis, the cost of i-FACTOR could theoretically be increased 70-fold and still remain cost-effective.Ĭonclusion: The novel i-FACTOR is not only cost-effective compared to autograft in ACDF surgery but is the dominant economic strategy. The ICER at 90 days was $13,333 per QALY and became negative (“dominated”) relative to the control group within one year and onwards. The savings proved to be incremental over time, increasing to 3.7% over an extrapolated 10 years. Results: In all scenarios, i-FACTOR reduced costs within the first year by 1.4% to 2.1%. Cost-effectiveness was expressed as an incremental cost-effectiveness ratio (ICER). Health-related utility outcome was expressed in quality-adjusted life years (QALYs). In the base-case analysis, both health and societal system costs were evaluated. Two primary outcome measures were assessed: cost and utility. We analyzed various real-world scenarios, including inpatient and outpatient surgical settings as well as private versus public insurances. Patients randomly received either autograft (N = 154) or i-Factor (N = 165).
#IFACTOR BONE GRAFT TRIAL#
Methods: The patient cohort was extracted from a prospective, multicenter randomized control trial (RCT) from twenty-two North American centers. To evaluate the cost-effectiveness of i-FACTOR compared to autograft for patients undergoing ACDF surgery. Cost-effectiveness of these innovations remains an often-overlooked aspect of this effort.

Objective: The efficacy and safety of traditional anterior cervical discectomy and fusion (ACDF) surgery has improved with the introduction of new implants and compounds. Study Design: We conducted decision analytical modeling using a Markov model to determine the ICER of i-factor compared to autograft in ACDF surgery. Neuronomics LLC, 7320 Woodlake Ave, Suite 215, West Hills, CA, 91307, USA (2018) Neurosurgery Vol-83(3): pages 377-384.Bart Thaci, 1 Randy Yee, 2 Kee Kim, 1 Amir Vokshoor, 2– 4 J Patrick Johnson, 5 Jared Ament 2– 5ġUniversity of California, Davis, Sacramento, CA, USA 2Neuronomics LLC, Los Angeles, CA, USA 3Neurosurgery & Spine Group, Los Angeles, CA, USA 4Institute of Neuro Innovation, Santa Monica, CA, USA 5Cedars Sinai Medical Center, Los Angeles, CA, USA i-FACTOR Bone Graft vs Autograft in Anterior Cervical Discectomy and Fusion: 2-Year Follow-up of the Randomized Single-Blinded Food and Drug Administration Investigational Device Exemption Study.

Arnold PM, Sasso RC, Janssen ME, Fehlings MG, Heary RF, Vaccaro AR, Kopjar B. Results of the Prospective Randomized Single-blinded Food and Drug Administration Investigational Device Exemption Study.
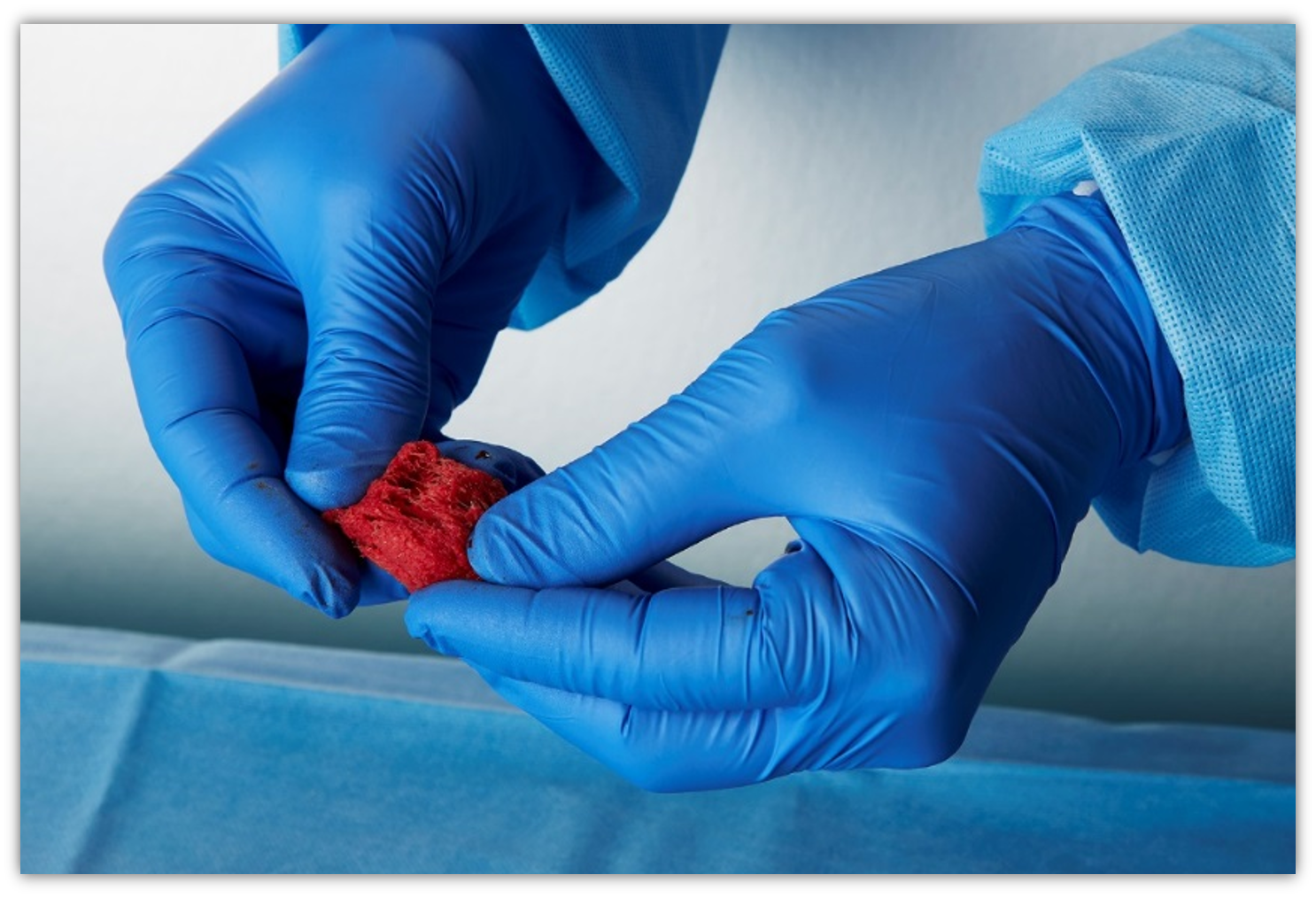
Efficacy of i-Factor™ Bone Graft versus Autograft in Anterior Cervical Disectomy and Fusion. Arnold PM, Sasso RC, Janssen ME, Fehlings MG, Smucker JD, Vaccaro AR, Heary RF, Patel AL, Goulet B, Kalfas IH, Kopjar B. Enhanced cell attachment to anorganic bone mineral in the presence of a synthetic peptide related to collagen. Biomimetic collagen scaffolds for human bone cell growth and differentiation. Enhanced cell attachment and osteoblastic activity by P-15 peptide-coated matrix in hydrogels. The effect of collagen 1 mimetic peptides on mesenchymal stem cells adhesion and differentiation, and on bone formation at hydroxyapatite surfaces.īiomaterials. Hennessy KM, Pollot BE, Clem WC, Phipps MC, Sawyer AA, Culpepper BK, Bellis SL.


 0 kommentar(er)
0 kommentar(er)
